When most people hear the word chlamydia, they are likely to think of the sexually transmitted disease caused by chlamydia trachomatis. But two other species of chlamydia bacteria are pathogenic to humans: C. psittaci and C. pneumoniae. Chlamydia pneumoniae (CPn) is a respiratory tract pathogen that causes pneumonia and can be transmitted from person to person through inhalation of airborne droplets or by touching infected surfaces and subsequently touching either the mouth or nose.
Recent research suggests that CPn bacteria are able to use the olfactory nerve in the nasal cavity to migrate to the brain and subsequently trigger a chronic neuroinflammatory response. Neuroinflammation alone is sufficient to damage and eventually kill neuron cells in the brain. But it may also lead to the production of beta-amyloid, the protein that forms the hallmark brain plaques seen in Alzheimer’s disease.1
In a population study in Taiwan, researchers found that patients infected with CPn exhibited a nearly 1.6-fold increased risk of developing AD in the following eight years compared to control subjects not infected with the bacteria.2 It was further shown that after treatment with a 15-day course of intravenous antibiotics, neuroinflammation, oxidative stress, and the formation of amyloid plaques were decreased and the risk of subsequent AD was attenuated.
Bacteria associated with periodontal disease also may lead to Alzheimer’s-related pathology. Scientists reported in the Journal of Alzheimer’s Disease an association between these bacteria, porphyromonas gingivalis, and risk of dementia. Periodontal disease develops when food particles and the bacteria form plaque on teeth which then irritates the gums causing inflammation and bleeding. Looking at records of 6,000 subjects who developed gum disease, researchers found that Alzheimer’s and death from AD in those 65 and older were associated with the presence of antibodies to P. gingivalis. In another study, tooth loss associated with severe gingivitis was associated with a 22 percent increased risk of Alzheimer’s.3
As in the case of CPn infection, the researchers found that the mouth bacteria, which can travel to the brain in the bloodstream, caused an inflammatory response and might trigger the production of beta-amyloid plaques.4 The CDC reports 47 percent of Americans aged 30 or older and 70 percent aged 65 and older have gum disease. While neither CPn nor P. gingivalis has been shown to be a cause of Alzheimer’s disease, the fact that these bacteria can infect the brain and activate pathological changes featured in the disease is cause for concern.
It’s been over 100 years since the first case of Alzheimer’s disease was diagnosed and we still lack a definitive understanding of its cause. However, it’s been estimated that up to 50 percent of Alzheimer’s cases worldwide result from just seven risk factors: diabetes, hypertension, obesity, smoking, depression, cognitive inactivity, and physical inactivity—all factors that are preventable and treatable.5 Periodontal disease is also preventable and treatable by maintaining good oral hygiene. If brain infection by CPn is conclusively shown to contribute to Alzheimer’s disease, then this risk factor, too, can be addressed by way of a vaccine to prevent infection. We may still be years away from discovering a cure for Alzheimer’s but science shows us there is much we can do today to dramatically lower risk of developing the disease.
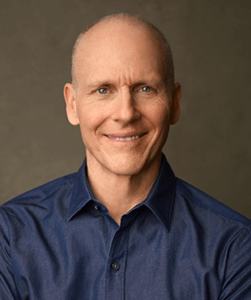
Joseph Keon is an investigative writer in the field of preventive medicine. He holds fitness expert certifications from both the Cooper Institute for Aerobics Research and the American Council on Exercise. In his work as a wellness consultant in the public and private sphere for over 20 years, Keon focused on chronic degenerative diseases and their relationship to modifiable lifestyle choices. He is a past member of the Board of Directors of the Wild Oats Wellness Foundation and Dr. Helen Caldicott’s Nuclear Policy Research Institute as well as the Marin Health Council, an advisory to the Marin County Board of Supervisors. Keon is currently a member of the American College of Lifestyle Medicine. Keon is the author of The Alzheimer’s Revolution as well as three other books including Whitewash: The Disturbing Truth about Cow’s Milk and Your Health.
1 Al-Atrache, Z., et al., “Astrocytes infected with Chlamydia pneumoniae demonstrate altered expression and activity of secretases involved in the generation of β-amyloid found in Alzheimer disease,” BMC Neuroscience (2019). doi.org/10.1186/s12868-019-0489-5
2 Hsun, Ou, et al., “Association Between Antibiotic Treatment of Chlamydia pneumoniae and Reduced Risk of Alzheimer Dementia: A Nationwide Cohort Study in Taiwan,” Frontiers in Aging Neuroscience (2021) doi.org/10.3389/fnagi.2021.701899
3 Demmer, Ryan T., et al., “Periodontal disease and incident dementia: The Atherosclerosis Risk in Communities Study (ARIC),” Neurology (2020). doi.org/10.1212/WNL.0000000000010312
4 Beydoun M, et al., “Clinical and bacterial markers of periodontitis and their association with incident all-cause and Alzheimer’s disease dementia in a large national survey,” Journal of Alzheimer’s Disease 75 (2020):157-172.
5 Barnes, Deborah E., “The projected impact of risk factor reduction on Alzheimer’s disease prevalence,” Lancet Neurology 10 (2011):819-28.